
General anesthesia remains the cornerstone of anesthesia practice; many surgical procedures cannot be done under regional techniques or monitored anesthesia care with sedation.
The induction of general anesthesia can precipitate catastrophic anesthetic complications. Many different techniques can be used to induce general anesthesia, each with significant advantages and disadvantages.
Intravenous induction, used primarily in adults, quickly produces unconsciousness, and depending on the agent used, apnea as well. Propofol, the most common induction agent currently used, can cause hypotension due to its myocardial depressing and vasodilatory properties. Hypertension and tachycardia commonly occur during laryngoscopy or other significant airway stimulation.
The goal of a rapid sequence induction (RSI) is to achieve secure protection of the airway with a cuffed endotracheal tube without ever mask ventilating a patient. It is intended to prevent vomiting and aspiration, and it is routinely employed in patients at heightened risk for aspiration. There are no randomized controlled trials that demonstrate any kind of outcome benefit of rapid sequence induction in such patients, but it is nevertheless routinely employed for this purpose in the United States.
Pediatric patients are often not amenable to preoperative IV catheter placement. Hence, inhalation induction of anesthesia is commonly used in children, with IV placement occurring after induction. Even among children, however, patients at heightened risk for aspiration or with a full stomach may be best managed with preoperative IV placement and an IV induction. Patients with developmental delay may not be amenable to preoperative IV placement or inhalational induction of anesthesia. In such patients, intramuscular administration of an agent such as ketamine is often required to induce anesthesia.
Airway Management
Most anesthesiologists prefer to secure the airway of a patient undergoing general anesthesia, and this is usually accomplished immediately after anesthesia has been induced. The airway may be managed in several ways, including by face mask, with a laryngeal mask airway (LMA), or, most definitively, by endotracheal intubation with a cuffed endotracheal tube. Nasal and oral airways can help establish a patent airway in a patient being ventilated with a mask by creating an air passage behind the tongue.
The LMA is a cuffed supraglottic oral airway that is inserted through the oropharynx and ideally positioned just above the glottis opening. It is passed blindly, and the inflated cuff creates a seal around the laryngeal inlet. An LMA does not protect against aspiration and should generally not be used in patients with a high risk of aspiration.
Tracheal intubation requires a skilled operator and proper equipment. In most elective anesthetics, attempts to intubate the trachea are facilitated by the administration of muscle relaxants in a patient who is already under a general anesthetic. Intubation is typically performed under direct visualization with a laryngoscope, watching the endotracheal tube pass through the vocal cords into the trachea. To obtain a direct line of sight, the patient is placed in the sniffing position. The neck is flexed at the lower cervical spine and extended at the atlanto-occipital joint. This flexion and extension are amplified during laryngoscopy. Laryngoscope blades can be curved (Macintosh) or straight (Miller) blades. Laryngoscopic views are typically reported in a classification system developed by Cormack and Lehane (Figure).
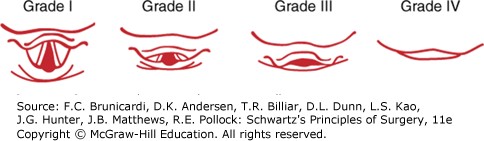
Figure legend: Laryngoscopic views obtained per Cormack and Lehane. Anesthesia for Surgical Patients, Brunicardi F, Andersen DK, Billiar TR, Dunn DL, Kao LS, Hunter JG, Matthews JB, Pollock RE. Schwartz's Principles of Surgery, 11e; 2019.
Board Review Questions
Choose the one best response to each question.
1. Potential side effect(s) of succinylcholine include
A. hyperkalemia
B. rhabdomyolysis
C. malignant hyperthermia
D. myalgias
E. all of the above
2. Patterns of nerve stimulation used to monitor neuromuscular function include
A. single twitch
B. train-of-four (TOF)
C. double-burst stimulation (DBS)
D. tetany
E. all of the above
3. The mechanism of action of local anesthetics is best described as
A. binding of the cationic form of the local anesthetic molecule to extracellular local anesthetic receptors
B. binding of the neutral (basic) form of the local anesthetic molecule to cytoplasmic receptors
C. binding of the cationic form of the local anesthetic molecule to transmembrane sodium receptors in the inactivated-closed state
D. binding of the neutral (basic) form of the local anesthetic molecule to transmembrane sodium channels in the activated-open state
E. binding of the local anesthetic molecule to transmembrane potassium channels
Answers
1. The correct answer is E. all of the above
2. The correct answer is E. all of the above
3. The correct answer is C. binding of the cationic form of the local anesthetic molecule to transmembrane sodium receptors in the inactivated-closed state

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.