
Hemostasis is a complex process whose function is to limit blood loss from an injured vessel. Four major physiologic events participate in the hemostatic process: vascular constriction, platelet plug formation, fibrin formation, and fibrinolysis. Although each tends to be activated in order, the four processes are interrelated so that there is a continuum and multiple reinforcements. The process is shown schematically in the figure.
Vasoconstriction: The extent of vasoconstriction varies with the degree of vessel injury. A small artery with a lateral incision may remain open due to physical forces, whereas a similarly sized vessel that is completely transected may contract to the extent that bleeding ceases spontaneously.
Platelet aggregation: Platelets do not normally adhere to each other or to the vessel wall but can form a plug that aids in cessation of bleeding when vascular disruption occurs. Injury to the intimal layer in the vascular wall exposes subendothelial collagen to which platelets adhere. This process requires von Willebrand factor (vWF), a protein in the subendothelium that is lacking in patients with von Willebrand’s disease. vWF binds to glycoprotein (GP) I/IX/V on the platelet membrane. Following adhesion, platelets initiate a release reaction that recruits other platelets from the circulating blood to seal the disrupted vessel.
Coagulation: The intrinsic pathway begins with the activation of factor XII that subsequently activates factors XI, IX, and VIII. In this pathway, each of the primary factors is “intrinsic” to the circulating plasma, whereby no surface is required to initiate the process. In the extrinsic pathway, tissue factor (TF) is released or exposed on the surface of the endothelium, binding to circulating factor VII, facilitating its activation to VIIa. Each of these pathways continues on to a common sequence that begins with the activation of factor X to Xa (in the presence of VIIIa). Subsequently, Xa (with the help of factor Va) converts factor II (prothrombin) to thrombin and then factor I (fibrinogen) to fibrin. Clot formation occurs after fibrin monomers are cross-linked to polymers with the assistance of factor XIII.
Fibrinolysis: Fibrin clot breakdown (lysis) allows restoration of blood flow during the healing process following injury and begins at the same time clot formation is initiated. Fibrin polymers are degraded by plasmin, a serine protease derived from the proenzyme plasminogen. Plasminogen is converted to plasmin by one of several plasminogen activators, including tPA. Plasmin then degrades the fibrin mesh at various places, leading to the production of circulating fragments, termed fibrin degradation products (FDPs), cleared by other proteases or by the kidney and liver.
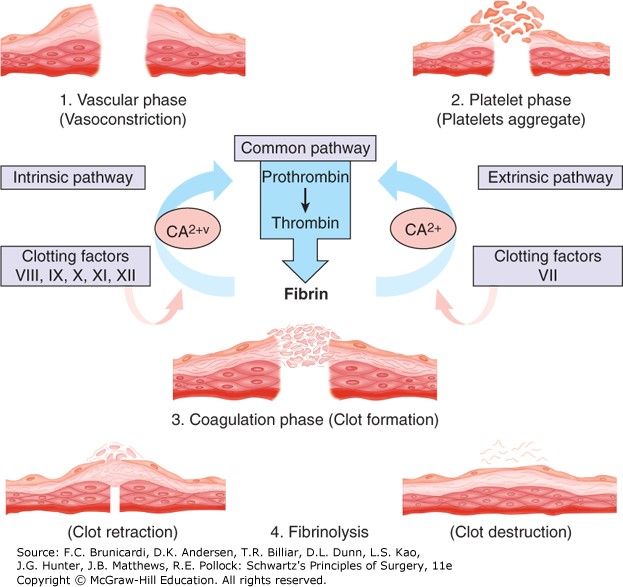
Figure legend: Biology of hemostasis. The four physiologic processes that interrelate to limit blood loss from an injured vessel are illustrated and include vascular constriction, platelet plug formation, fibrin clot formation, and fibrinolysis.
Board Review Questions
1. Which of the following is NOT one of the four major physiologic events of hemostasis?
A. Fibrinolysis
B. Vasodilatation
C. Platelet plug formation
D. Fibrin production
2. Which is required for platelet adherence to injured endothelium?
A. Thromboxane A2
B. Glycoprotein (GP) IIb/IIIa
C. Adenosine diphosphate (ADP)
D. Von Willebrand factor (vWF)
3. In a previously unexposed patient, when does the platelet count fall in heparin-induced thrombocytopenia (HIT)?
A. <24 hours
B. 24–28 hours
C. 3–4 days
D. 5–7 days
Answers
1. The correct answer is B. Vasodilatation
2. The correct answer is D. Von Willebrand factor (vWF)
3. The correct answer is D. 5–7 days

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.