
Unlike in the other vascular beds, symptoms of extracranial carotid disease are most often caused by embolization. Arterial emboli account for approximately one-quarter of strokes in Europe and North America, and 80% of these originate from atherosclerotic lesions in a surgically accessible artery in the neck. The most common lesion is at the bifurcation of the carotid artery. Transcranial Doppler studies have shown that emboli are seen in approximately 20% of patients with moderate (> 50% stenosis) lesions at the carotid bifurcation and even higher rates with more than 70% stenoses. The incidence and frequency of emboli are increased in recently symptomatic patients.
The neurologic dysfunction associated with microemboli may appear as sudden “short-lived,” or transient, neurologic symptoms that may include unilateral motor and sensory loss, aphasia (difficulty with understanding and expressing language), or dysarthria (difficulty speaking due to motor dysfunction). These are termed transient ischemic attacks (TIAs). Most TIAs are brief, but by convention, a duration of 24 hours is the limit of a TIA. If the symptoms persist, it is a stroke, or cerebrovascular accident (CVA). An embolus to the ophthalmic artery, the first branch of the internal carotid artery, produces a temporary monocular loss of vision called amaurosis fugax or permanent blindness. Atherosclerotic emboli may be visible as small bright flecks (Hollenhorst plaques) lodged in arterial bifurcations in the retina.
Characteristically, lesions of atherosclerosis in the internal carotid artery occur along the wall of the carotid bulb opposite to the external carotid artery origin (Figure 36–10). The enlargement of the bulb just distal to this major branch point creates an area of low wall shear stress, flow separation, and loss of unidirectional flow. Presumably, this allows greater interaction of atherogenic particles and the vessel walls at this site and accounts for the localized plaque at the carotid bifurcation.
The accessibility of this localized atheroma allows effective removal of the plaque and a dramatic reduction in stroke risk. Landmark trial data from the 1990s demonstrated that with even the best medical therapy at that time, 26% of patients with TIAs and 70% or greater stenosis of the carotid artery develop permanent neurologic impairment (CVA) from continued embolization at 2 years. The risk of CVA can be reduced to 9% with plaque removal. The risk of CVA is lower for patients presenting with amaurosis fugax.
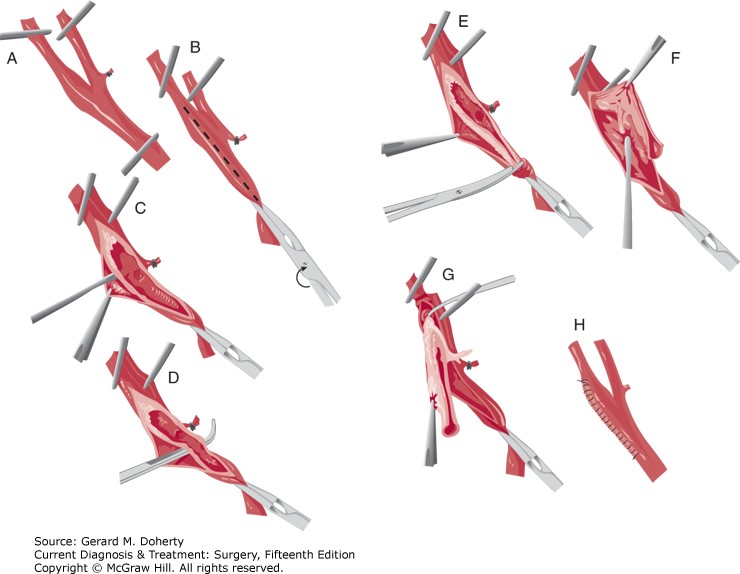
Figure Legend: Technique of carotid endarterectomy. Arteries, Doherty GM. Current Diagnosis & Treatment: Surgery, 15e; 2020.
Board Review Questions
1. A 22-year-old male presents to the ER after being struck in the neck with a baseball bat. Initial vitals include GCS 15, pulse rate 96 bpm, respiration rate 16 breaths/min, and SBP 125. An arteriogram is performed and reveals a right internal carotid artery dissection.
Initial management includes all the following except:
A. Cervical spine x-rays
B. Heparin
C. Neck exploration with repair
D. CT scan of the neck
E. Tracheobronchoscopy
2. Carotid endarterectomy
A. Should not be performed when the carotid artery is completely occluded
B. Has not been shown to be beneficial for any patients in prevention of ipsilateral stroke
C. Is performed through a catheter placed in the ipsilateral femoral artery
D. Carries a 30% risk of transient cranial nerve injury
E. Has a restenosis rate of 35% at 5 years
3. Arterial occlusive disease
A. Occurs predominantly due to congenital abnormalities or anatomical anomalies
B. Includes disease caused by atherosclerotic plaques, which typically develop at arterial branch points of high shear stress
C. Is masked by collateral arterial circulation that typically has a lower resistance than the original unobstructed artery
D. Typically occurs with at least a 50% reduction in arterial diameter, which correlates with a 75% narrowing of cross-sectional area
E. Causes symptoms due to high pressure proximal to stenosis
Answers
1. The correct answer is C. Neck exploration with repair
2. The correct answer is A. Should not be performed when the carotid artery is completely occluded
3. The correct answer is D. Typically occurs with at least a 50% reduction in arterial diameter, which correlates with a 75% narrowing of cross-sectional area

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.