
Acute pancreatitis is an inflammatory disease of the pancreas that is associated with little or no fibrosis of the gland. It can be initiated by several factors including gallstones, alcohol, trauma, and infections, and in some cases it is hereditary. Very often patients with acute pancreatitis develop additional complications such as sepsis, shock, and respiratory and renal failure, resulting in considerable morbidity and mortality. Approximately 300,000 cases occur in the United States each year, 10 to 20% of which are severe, leading to over 3000 deaths. Pancreatitis is a contributing factor in an additional 4000 deaths annually and inflicts a heavy economic burden accounting for more than $2 billion in health costs annually in the U.S.
Etiology
The etiology of acute pancreatitis is a complex subject because many different factors have been implicated in the causation of this disease, and sometimes there are no identifiable causes. Two factors, biliary tract stone disease and alcoholism, account for 80 to 90 percent of the cases. The remaining 10 to 20 percent is accounted for either by idiopathic disease or by a variety of miscellaneous causes including trauma, surgery, drugs, heredity, infection and toxins.
Acute pancreatitis occurs in varying degrees of severity, the determinants of which are multifactorial. The generally prevalent belief today is that pancreatitis begins with the activation of digestive zymogens inside acinar cells which cause acinar cell injury. Recent studies suggest that the ultimate severity of the resulting pancreatitis may be determined by the events that occur subsequent to acinar cell injury. These include inflammatory cell recruitment and activation, as well as generation and release of cytokines and other chemical mediators of inflammation.
Diagnosis
The clinical diagnosis of pancreatitis is one of exclusion. The other upper abdominal conditions that can be confused with acute pancreatitis include perforated peptic ulcer, a gangrenous small bowel obstruction, and acute cholecystitis. Since these conditions often have a fatal outcome without surgery, urgent intervention is indicated in the small number of cases in which doubt persists.
All episodes of acute pancreatitis begin with severe pain, generally following a substantial meal. The pain is usually epigastric, but can occur anywhere in the abdomen or lower chest. It has been described as "knifing" or "boring through" to the back, and may be relieved by the patient leaning forward. It precedes the onset of nausea and vomiting, with retching often continuing after the stomach has emptied. Vomiting does not relieve the pain, which is more intense in necrotizing than in edematous pancreatitis. An episode of acute pancreatic inflammation in a patient with known chronic pancreatitis has the same findings.
On examination the patient may show tachycardia, tachypnea, hypotension, and hyperthermia. The temperature is usually only mildly elevated in uncomplicated pancreatitis. Voluntary and involuntary guarding can be seen over the epigastric region. The bowel sounds are decreased or absent. There are usually no palpable masses. The abdomen may be distended with intraperitoneal fluid. There may be pleural effusion, particularly on the left side.
With increasing severity of disease, the intravascular fluid loss may become life-threatening as a result of sequestration of edematous fluid in the retroperitoneum. Hemoconcentration then results in an elevated hematocrit. However, there also may be bleeding into the retroperitoneum or the peritoneal cavity. In some patients (about 1%), the blood from necrotizing pancreatitis may dissect through the soft tissues and manifest as a blueish discoloration around the umbilicus (Cullen's sign) or in the flanks (Grey Turner sign). The severe fluid loss may lead to prerenal azotemia with elevated blood urea nitrogen and creatinine levels. There also may be hyperglycemia, hypoalbuminemia, and hypocalcemia sufficient in some cases to produce tetany.
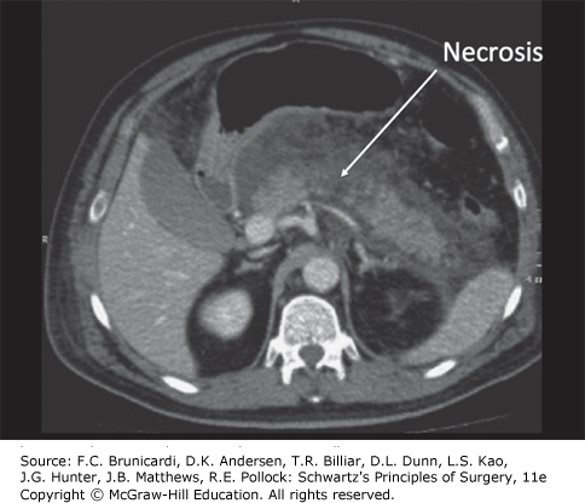
Computed tomography scan showing well perfused interstitial edematous acute pancreatitis of the neck and tail of the pancreas with a confluent area of necrosis of the pancreatic body. The pancreas is surrounded by fluid, inflammation, and possible peripancreatic fat necrosis.
Board Review Questions
1. Which is true about the surgical anatomy of the pancreas?
A. The head lies over the first lumbar vertebra.
B. The accessory duct enters the second part of the duodenum.
C. The superior mesenteric vessels pass behind the uncinate process.
D. The SMA lies to the left of the superior mesenteric vein.
E. The superior mesenteric vein joins the portal vein behind the head of the pancreas.
2. A 10-year-old child develops severe abdominal pain while in the hospital for a viral syndrome. The pain is better if she sits up and leans forward, laboratory studies demonstrate an amylase of 180 and WBC of 15,000. CT scan of the abdomen demonstrates an edematous pancreatic gland and retroperitoneal stranding. What is the most likely cause for her pancreatitis?
A. Gallstone pancreatitis
B. Coxsackie virus infection
C. Heterotopic pancreas
D. Drug-induced pancreatitis
E. Spherocytosis
3. Which of the following is the most commonly used initial treatment for pancreatic ascites?
A. Octreotide, bowel rest, TPN
B. Endoscopic stenting of the pancreatic duct
C. Roux-en-Y pancreaticojejunostomy
D. Distal pancreatectomy
Answers
1. The correct answer is D. The SMA lies to the left of the superior mesenteric vein
2. The correct answer is B. Coxsackie virus infection
3. The correct answer is A. Octreotide, bowel rest, TPN

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.