
There are three pairs of major salivary glands (parotid, submandibular, and sublingual) responsible for the secretion of saliva and stimulated by swallowing. Hundreds of minor salivary glands maintain resting levels of saliva necessary for moisturizing, lubrication, cleansing, digestion, and immunologic protection of the mouth.
Acute Bacterial Sialadenitis
Acute bacterial sialadenitis may develop secondary to obstruction, stasis of saliva, or decreased secretion. There is diffuse painful enlargement of the gland, often with erythema and tenderness. Typically this occurs in the older patient who is taking diuretics or is dehydrated. The most common organism responsible, especially in acute parotitis, is S aureus. Other organisms include streptococci, E coli, and anaerobes. Antibiotic therapy is with a first-generation cephalosporin (cephalothin or cephalexin) or dicloxacillin. Alternatives are clindamycin, amoxicillin-clavulanate, or ampicillin-sulbactam.
Viral Sialadenitis
Mumps is the most common viral cause of acute salivary inflammation. Young children 4–10 years of age are most commonly affected, developing bilateral swelling of the parotid glands 2–3 weeks after exposure. Symptoms last 7–10 days. Cytomegalovirus (CMV) is the second most common cause of acute viral sialadenitis and may mimic infectious mononucleosis clinically and hematologically.
Chronic Sialadenitis
Chronic or recurrent bacterial sialadenitis or submandibular sialadenitis may develop as a result of antecedent acute suppuration or viral inflammation. More commonly, however, there is a history of ductal obstruction. Recurrent bacterial invasion of the parotid gland or submandibular gland leads to destruction and fibrosis of acini with ductal ectasia. The subsequent decrease in salivary flow creates a cycle of ascending sialadenitis, ductal ectasia, acinar atrophy, and obstructive fibrosis. Clinically, the patient complains of recurrent parotid pain and swelling, typically while eating. Initial treatment should be conservative, utilizing sialagogues (lemon balls or chewing gum), adequate oral hydration to stimulate salivary flow, and amoxicillin-clavulanate or cephalexin. In patients with recalcitrant disease, an extended course of clindamycin, cefoxitin, nafcillin, or vancomycin plus metronidazole may be necessary if methicillin-resistant S aureus and penicillin-resistant streptococci are considered. Superficial parotidectomy is recommended if prolonged conservative management fails.
SIALOLITHIASIS
Salivary gland stones are both a cause and a consequence of chronic sialadenitis. In addition, they may produce acute suppurative sialadenitis. The stones are composed of inorganic calcium and sodium phosphate salts that are deposited in the duct on an organic nidus of mucus or cellular debris. Eighty to ninety percent of salivary calculi occur in the submandibular gland and may lead to complete acute obstruction of the gland, with most stones occurring in the ducts rather than the gland itself. The patient complains of painful swelling, especially with meals, and may report extrusion of gravel from the duct.
The diagnosis is confirmed by palpation of a stone or by demonstration of decreased salivary flow from the duct. Soft tissue films may reveal a radiodense stone, and CT may show sialoliths, though 20–40% of calculi are radiolucent on plain films. Treatment consists of intraoral removal of stones that are close to the duct orifice by ductal dilation and massage. Stones in the hilum of the submandibular gland necessitate excision of the gland if associated with chronic pain and swelling. Parotid sialoliths are managed in a similar fashion.
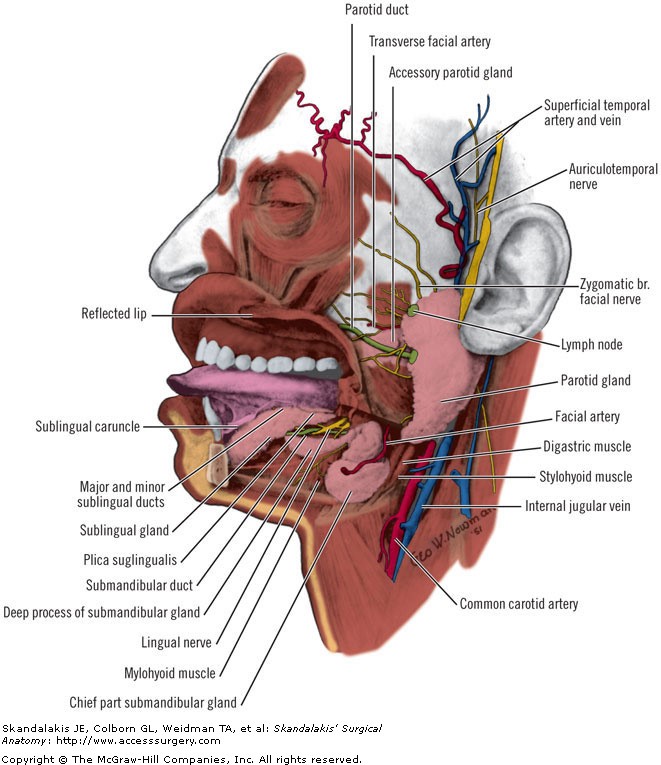
Figure legend: Salivary glands and their ducts. Dissection showing the sublingual, submandibular (submaxillary), and parotid glands. Deep lateral view of the lingual region with the body and part of the ramus of the mandible cut away to expose the glands and related structures. (Modified from Anson BJ (ed). Morris' Human Anatomy (12th ed). New York: McGraw-Hill, 1966; with permission.)
Board Review Questions
1. A 19-year-old woman presents to the ER with few days history of fever and pain in the submandibular region. She says that over the last several hours she has been having more trouble speaking with pain in her tongue and is afraid to lie down. On oral examination, you see that the floor of mouth is indurated and swollen and very tender. The patient has very poor dentition but you do not appreciate an abscess. Her submandibular and submental regions are also tender and indurated with some fluctuance. What entity in the differential diagnosis are you most worried about?
A. Vincent’s angina
B. Bezold’s abscess
C. Ludwig’s angina
D. A retropharyngeal abscess
E. Submandibular and sublingual gland sialadenitis
2. An 80-year-old woman who is a nursing home patient is brought to the hospital with a GI bleed. She ultimately undergoes a left hemicolectomy for diverticulosis and has a lengthy postoperative ileus. Postoperative day 5 she complains of a sour taste in her mouth and her right cheek feeling warm and very tender. You notice a swelling in the parotid area and that she is febrile at the time. All of the following would be part of the treatment of this disorder except
A. IV antibiotics against S. aureus
B. Heat application to the area over the parotid
C. IV hydration
D. Lemon drops
E. Cannulation of the right Stensen’s duct with drainage
3. A 10-year-old girl presents with a solitary left-sided submandibular neck mass that has been present for a month. It is nontender and initially grew over the course of 2-3 days and then has not grown further. The most likely etiology of this mass is
A. Reactive lymph node
B. Atypical mycobacterial infection
C. Branchial cleft cyst
D. Submandibular gland sialadenitis
E. Lymphoma
Answers
1. The correct answer is C. Ludwig’s angina
2. The correct answer is E. Cannulation of the right Stensen’s duct with drainage
3. The correct answer is A. Reactive lymph node

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.