
Multisystem trauma, thermal burns, retroperitoneal injuries, and surgery related to the retroperitoneum are the major initial causative factors that may lead to abdominal compartment syndrome (ACS). Ruptured AAA, major pancreatic injury and resection, or multiple intestinal injuries are also examples of clinical situations in which a large volume of IV fluid resuscitation puts these patients at risk for intra-abdominal hypertension. Manifestations of ACS typically include progressive abdominal distention followed by increased peak airway ventilator pressures, oliguria followed by anuria, and an insidious development of intracranial hypertension. These findings are related to elevation of the diaphragm and inadequate venous return from the vena cava or renal veins secondary to the transmitted pressure on the venous system.
Measurement of abdominal pressures is easily accomplished by transducing bladder pressures from the urinary catheter after instilling 100 mL of sterile saline into the urinary bladder. A pressure greater than 20 mmHg constitutes intra-abdominal hypertension, but the diagnosis of ACS requires intra-abdominal pressure greater than 25 to 30 mmHg, with at least one of the following: compromised respiratory mechanics and ventilation, oliguria or anuria, or increasing intracranial pressures.
The treatment of ACS is to open any recent abdominal incision to release the abdominal fascia or to open the fascia directly if no abdominal incision is present. Immediate improvement in mechanical ventilation pressures, intracranial pressures, and urine output is usually noted. When expectant management for ACS is considered in the OR, the abdominal fascia should be left open and covered under sterile conditions (e.g., a vacuum-assisted open abdominal wound closure system) with plans made for a second-look operation and delayed fascial closure. Patients with intra-abdominal hypertension should be monitored closely with repeated examinations and measurements of bladder pressure, so that any further deterioration is detected and operative management can be initiated. Left untreated, ACS may lead to multiple system end-organ dysfunction or failure and has a high mortality.
Abdominal wall closure should be attempted every 48 to 72 hours until the fascia can be reapproximated. If the abdomen cannot be closed within 5 to 7 days following release of the abdominal fascia, a large incisional hernia is the net result. A variety of surgical options have evolved for prevention and closure of the resultant hernias, but no standard approach has yet evolved.
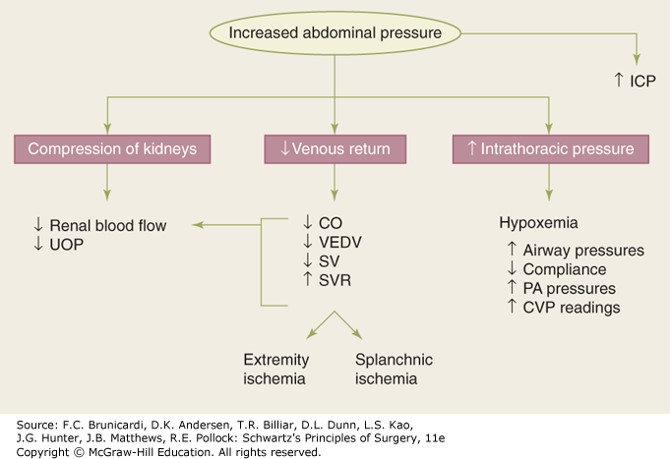
Figure legend: Abdominal compartment syndrome is defined by the end organ sequelae of intra-abdominal hypertension. CO = cardiac output; CVP = central venous pressure; ICP = intracranial pressure; PA = pulmonary artery; SV = stroke volume; SVR = systemic vascular resistance; UOP = urine output; VEDV = ventricular end diastolic volume.
Board Review Questions
1. The diagnosis of abdominal compartment syndrome is made with a bladder pressure greater than
A. >20 mm Hg
B. 40 mm Hg
C. 60 mm Hg
D. 80 mm Hg
2. Damage control surgery (DCS)
A. Limits enteric spillage by rapid repair of partial small bowel injuries with whipstitch, and complete transection with a GIA stapling device.
B. Aims to control surgical bleeding and identify injuries that can be managed conservatively or with interventional radiology.
C. Is indicated when patients develop intraoperative refractory hypothermia, serum pH >7.6, or refractory coagulopathy.
D. Abdominal wall should be closed with penetrating towel clips.
3. A 41-year-old male is shot in the abdomen multiple times undergoes an extensive exploratory laparotomy with multiple bowel resections. Following surgery, he is taken to the ICU for further resuscitation. Which of the following signs would not be consistent with the development of an abdominal compartment syndrome (ACS)?
A. Increasing peak airway pressures
B. Increasing bladder pressures
C. Decreasing cardiac output
D. Decreasing PCO2
E. Decreasing urine output under 15/h
Answers
1. The correct answer is A. >20 mm Hg
2. The correct answer is A. Limits enteric spillage by rapid repair of partial small bowel injuries with whipstitch, and complete transection with a GIA stapling device.
3. The correct answer is D. Decreasing PCO2

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.