NAPLEX Question of the Week: DVT Dosing Dilemma

KA is a 37-year-old female who presented to the emergency department with unilateral swelling, erythema, and tenderness in her left lower extremity. Her PMH is significant for depression, and her family history is significant for Factor V Leiden mutation. She denies feeling any chest tightness/pain, SOB, or dyspnea. Her doppler ultrasonography reveals a DVT in her leg, and her chest CTA was negative for PE.
SH: Smokes ½ ppd, denies alcohol use
Medications: Prozac 20 mg QD, Blisovi Fe 1.5 mg/30 mcg QD
Pertinent Labs:
BP: 127/81
HR: 77
Weight: 155 lbs
Height: 5’7”
D-Dimer: 1500 ng/mL
CrCl: 120 mL/min
Which of the treatment regimens are correct for the initial treatment of her DVT? Select all that apply.
A. Pradaxa 150mg PO BID
B. Xarelto 15 mg PO BID
C. Lovenox 70mg SQ once daily
D. Enoxaparin 40 mg SQ once daily
E. Coumadin 5 mg PO once daily
F. Eliquis 10mg PO BID
Correct Answers: B and F
Brand Generics: Prozac (fluoxetine), Blisovi (ethinyl estradiol and norethindrone), Xarelto (rivaroxaban), Eliquis (apixaban), Coumadin (warfarin), Lovenox (enoxaparin), Pradaxa (dabigatran)
Rationale: When first looking at this DVT case it is important to take notice of the patient’s signs/symptoms, history, labs, and risk factors. This patient was experiencing unilateral swelling, pain and redness in her leg and has an elevated D-dimer which are all classic signs of a DVT. In addition, she does have a family history of Factor V Leiden disease (genetic mutation that leads to factor V resistance to activated protein C, a natural anticoagulant) and a social history of smoking. Both factors put her at an increased risk of clot formation. In addition, she is on an oral contraceptive that contains estrogen which further amplifies her clot risk.
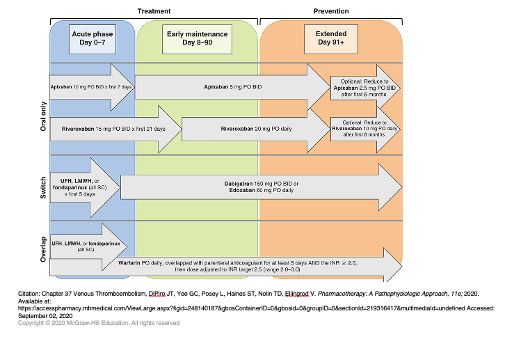
For treatment of DVT patients are typically started on parenteral anticoagulants (heparin, LMWH or fondaparinux) or oral agents (rivaroxaban, apixaban). Some agents may be started alongside parenteral anticoagulants known as bridging (e.g. warfarin). The initial treatment phase lasts around 7 days but ultimately depends on the agent/regimen used. The long-term phase of treatment will last for a minimum of 3 months and often 6-12 months depending on risk factors and whether the DVT/PE was provoked (e.g. long car ride) or unprovoked (no identifiable cause). For patients like the one in this case, modifiable risk factors should also be discussed. She may need to be counseled on smoking cessation and switched to non-estrogen containing contraception long-term.
Answer Choice A: This answer choice is incorrect. While this is the correct dose and frequency when using Pradaxa for DVT/PE, it cannot be given initially as 5 days of either LMWH or UFH should be given first before transitioning to Pradaxa therapy.
Answer Choice B: This is correct. Rivaroxaban can be used alone to treat DVT, and this is the dosing regimen recommended in the guidelines. The dose starts at 15 mg PO BID and then decreases to 20 mg PO QD after 21 days.
Answer Choice C: This answer is incorrect because the dose of enoxaparin used is too low. 1 mg/kg SQ QD (70mg) is the correct renally adjusted dose for patients with a CrCl < 30 mL/min. This patient has normal kidney function (CrCl= 120 mL/min) so she should be on 1.5 mg/kg SQ QD or 1 mg/kg SQ Q12H for treatment dosing.
Answer Choice D: This answer is incorrect because this is the DVT prophylaxis dose of enoxaparin. Treatment doses for enoxaparin are 1.5 mg/kg SQ QD or 1 mg/kg SQ Q12H as stated above.
Answer Choice E: This answer is incorrect because warfarin cannot be started alone to initially treat DVT. Warfarin must be overlapped with either UFH, a LMWH or fondaparinux for at least 5 days and the INR must be > 2 before it can be used alone. Once these goals are met, the patient may be continued on warfarin monotherapy with the dose adjusted to a goal INR of 2-3.
Answer Choice F: This answer choice is correct. Apixaban may be used alone to treat DVT, and 10 mg PO BID x 7 days followed by 5 mg PO BID is the correct dosing regimen.
Exam Competencies: Area 1 – Obtain, Interpret, or Assess Data, Medical, or Patient Information (1.4 – From medical records: treatment adherence, or medication-taking behavior; chief complaint, medication history, medical history, family history, social history, lifestyle habits, socioeconomic background; 1.5 – Signs or symptoms of medical conditions, healthy physiology, etiology of diseases, or pathophysiology), Area 2 – Identify Drug Characteristics (2. 1 – Pharmacology, mechanism of action, or therapeutic class), Area 3 – Develop or Manage Treatment Plans (3.4 – Drug dosing or dosing adjustments; duration of therapy)
Guidelines of Note: 2012 CHEST VTE Treatment Guidelines, 2016 CHEST VTE Treatment Guideline Update, 2021 CHEST VTE Treatment Guideline Update
Helpful Chart Detailing Various Treatment Regimens

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.