
Cerebrovascular disease is the most frequent cause of new rapid-onset, nontraumatic neurologic deficit. It is a far more common etiology than seizures or tumors. Vascular structures are subject to a variety of chronic pathologic processes which compromise vessel wall integrity. Diabetes, high cholesterol, high blood pressure, and smoking are risk factors for vascular disease. These conditions can lead to vascular damage by such mechanisms as atheroma deposition causing luminal stenosis, endothelial damage promoting thrombogenesis, and weakening of the vessel wall resulting in aneurysm formation or dissection. These processes may coexist. For instance, a vessel may contain an atheromatous plaque that significantly decreases lumen diameter, and also have compromised endothelium over the plaque, providing the opportunity for thrombus formation, which can lead to acute total occlusion of the remaining lumen. Aneurysms and dissection often occur in atheromatous vessels. Specific patterns of disease relevant to the cerebrovascular system are atheromatous and thrombotic carotid occlusion, brain ischemia due to embolus from a proximal source, vessel wall breakage leading to hemorrhage, and rupture of abnormal, thin-walled structures, specifically aneurysms and arteriovenous malformations.
Ischemic Diseases
Ischemic stroke accounts for approximately 85% of acute cerebrovascular events. Symptoms of acute ischemic stroke vary based on the functions of the neural tissues supplied by the occluded vessel, and the presence or absence of collateral circulation. The circle of Willis provides extensive collateral circulation, as it connects the right and left carotid arteries to each other and each to the vertebrobasilar system. Patients with complete occlusion of the carotid artery proximal to the circle of Willis may be asymptomatic if the blood flow patterns can shift and provide sufficient circulation to the ipsilateral cerebral hemisphere from the contralateral carotid and the basilar artery. However, the anatomy of the circle of Willis is highly variable. Patients may have a hypoplastic or missing communicating artery, both anterior cerebral arteries supplied by one carotid, or the posterior cerebral artery supplied by the carotid rather than the basilar. Similarly, one vertebral artery is often dominant, and the other hypoplastic. These variations may make disease in a particular vessel more neurologically devastating than in a patient with full collateral circulation. Occlusion distal to the circle of Willis generally results in stroke in the territory supplied by the particular artery.
Neurologic deficit from occlusive disease may be temporary or permanent. A patient with sudden-onset focal neurologic deficit that resolves within 24 hours has had a transient ischemic attack (TIA). If the deficit resolves between 24 hours and 1 week, then the patient has had a reversible ischemic neurologic deficit (RIND). A patient with permanent deficits has had a cerebrovascular accident (CVA). CVA is a commonly used, but vague term. Some prefer the term completed stroke.
Thrombotic Disease
The most common area of neurologically significant vessel thrombosis is the carotid artery in the neck. Disease occurs at the carotid bifurcation. Thrombosis of a carotid artery chronically narrowed by atheroma can lead to acute carotid occlusion. As discussed above, this may or may not cause symptoms. The more common concern is thromboembolus. Intracranial arterial occlusion by local thrombus formation may occur, but is considered rare compared to embolic occlusion.
Management
Complete occlusion of the carotid artery without referable neurologic deficit requires no treatment. A patient with new neurologic deficit and an angiographically demonstrated complete carotid occlusion contralateral to the symptoms should be considered for emergency carotid endarterectomy.11 Surgery should not be performed on obtunded or comatose patients, and should be done within 2 hours of symptom onset. This time restriction significantly reduces the number of candidates.
Embolic Disease
Emboli causing strokes may originate in the left atrium due to atrial fibrillation, on a hypokinetic left ventricular wall segment, or in valvular vegetations, an atheromatous aortic arch, or stenosed carotid bifurcations, or from the systemic venous system in the presence of a right-to-left shunt, such as a patent foramen ovale. The majority of emboli enter the anterior (carotid) circulation rather than the posterior (vertebrobasilar) circulation. Characteristic clinical syndromes result from embolic occlusion of the various vessels.
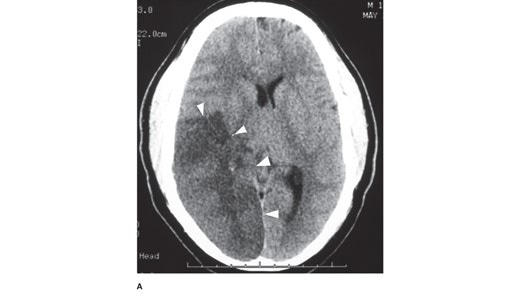
Figure legend: A. Head computed tomography scan of a patient with a 4-day-old stroke that occluded the right middle cerebral and posterior cerebral arteries. The infarcted tissue is the hypodense (dark) area indicated by the arrowheads. The patient presented with left-sided weakness and left visual field loss, but then became less responsive, prompting this head computed tomography. Note the right-to-left midline shift. Neurosurgery, Brunicardi F, Andersen DK, Billiar TR, Dunn DL, Kao LS, Hunter JG, Matthews JB, Pollock RE. Schwartz's Principles of Surgery, 11e; 2019.
Board Review Questions
1. Which of the following statements concerning patients who have an asymptomatic bruit located at the carotid bifurcation is true?
A. Approximately 50% of these bruits originate in the external carotid artery
B. The loudest bruits are heard when the stenosis is tightest
C. If these patients develop symptoms, transient ischemic attacks usually precede frank strokes
D. Almost 50% of these patients will develop neurologic symptoms within 5 years
2. A 60-year-old man has had recurrent episodes of amaurosis fugax and hemiparesis for the last year. Which of the following measures would be LEAST helpful in the workup of this man’s disorder?
A. Electrocardiography
B. Cerebral blood flow studies
C. Doppler flow studies
D. Computed tomography scan of the head
3. Which of the following is a risk factor specific for peripheral vascular disease?
A. Family history
B. Hyperhomocysteinemia
C. Elevated high-density lipoprotein (HDL)
D. Elevated low-density lipoprotein (LDL)
Answers
1. The correct answer is D. Almost 50% of these patients will develop neurologic symptoms within 5 years
2. The correct answer is D. Computed tomography scan of the head
3. The correct answer is B. Hyperhomocysteinemia

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.