
An estimated 46,420 patients developed pancreatic cancer in the United States in 2014, and 39,590 died of the disease. These nearly equal numbers illustrate the dismal prognosis generally associated with pancreatic carcinoma. The death rate per 100,000 people has been basically unchanged since the mid 1960s at about 10/100,000 for men and 27/100,000 for women. After tumors of the lung, prostate and colon, pancreatic carcinoma is the fourth leading cause of death due to cancer in men, and trails lung, breast and colon in women. Factors associated with an increased risk of pancreatic cancer are cigarette smoking, dietary consumption of meat (especially fried meat) and fat, previous gastrectomy (> 20 years earlier), and race. The incidence in Western Europe is similar to that in the United States and has also remained stable during the past three decades. In Europe, pancreatic cancer is the sixth leading cause of cancer death. In Japan, however, a dramatic increase has been observed during the last three decades, although the overall incidence is still less than that observed in the West. The lowest incidence worldwide is seen in parts of the Middle East and in India. Worldwide over 200,000 people die annually of cancer of the pancreas.
The percentage of patients with pancreas and other periampullary cancers that survive 5 years or longer after resection is dependent on multiple factors including site of primary and the stage of disease. The mean survival following palliative therapy is 7 months. Following a Whipple procedure, survival averages about 18 months. Factors associated with tumor recurrence and shorter survival include lymph node involvement, tumor size over 2.5 cm, blood vessel invasion, and amount of blood transfused. If tumor cells extend to the margins of the resected specimen, long-term survival is rare. If the margins are clear, about 20% of patients live more than 5 years. Overall 5-year survival is about 10%, but only 60% of these patients are actually free of tumor.
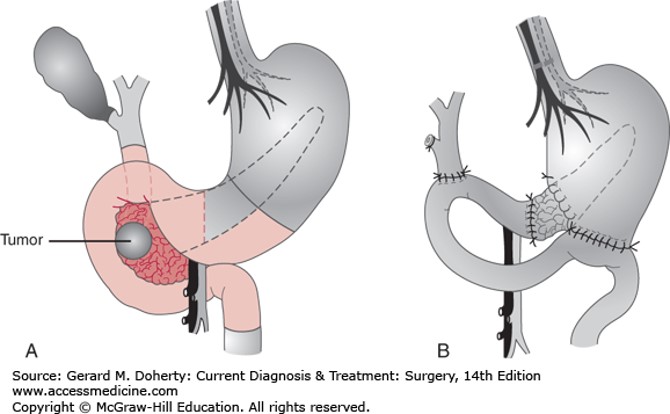
Pancreaticoduodenectomy (Whipple procedure). A: Preoperative anatomic relationships showing a tumor in the head of the pancreas. B: Postoperative reconstruction showing pancreatic, biliary, and gastric anastomoses. A cholecystectomy and bilateral truncal vagotomy are also part of the procedure. In many cases, the distal stomach and pylorus can be preserved, and vagotomy is then unnecessary.
Board Review Questions
1. Which is of the following statements about pancreatic adenocarcinoma is false?
A. The 5-year survival for pancreatic cancer is less than 5%
B. The yearly U.S. incidence of pancreatic cancer is approximately 45,000 cases
C. Familial predisposition and chronic pancreatitis are both risk factors for developing pancreatic cancer
D. There is no association between cigarette smoking and pancreatic cancer
E. Pain, jaundice, and weight loss are the most common presenting signs of pancreatic cancer
2. What is the most common mode of presentation of intraductal papillary mucinous tumors (IPMT) affecting the main pancreatic duct?
A. Recurrent episodes of abdominal pain and pancreatitis
B. Incidental pancreatic nodule found on CT
C. Atypia of ERCP brushings
D. Asymptomatic
E. No characteristic presentation
3. Which of the following is true with regard to palliative strategies for unresectable pancreatic cancer?
A. Advanced pancreatic adenocarcinoma is rarely a symptomatic disease
B. Celiac axis neurolysis is effective in 90% of patients over the short term
C. Gastric outlet obstruction (GOO) in the presence of unresectable disease is best treated by gastrojejunostomy
D. Presence of biliary obstruction is best treated with biliary-enteric anastomosis
E. Prophylactic gastrojejunal anastomosis is widely recommended
Answers
1. The correct answer is D. There is no association between cigarette smoking and pancreatic cancer
2. The correct answer is A. Recurrent episodes of abdominal pain and pancreatitis
3. The correct answer is C. Gastric outlet obstruction (GOO) in the presence of unresectable disease is best treated by gastrojejunostomy

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.