
Nutrition Requirements & Substrates
The body requires an energy source to remain in steady state. About 50% of the basal metabolic rate (BMR) reflects the work of ion pumping, 30% represents protein turnover, and the remainder represents recycling of amino acids, glucose, lactate, and pyruvate. Total energy expenditure is the sum of energy consumed in basal metabolic processes, physical activity, the specific dynamic action of protein, and extra requirements resulting from injury, sepsis, or burns.
Energy consumed in physical activity constitutes 10–50% of the total in normal subjects but decreases to 10–20% for hospitalized patients. Energy expenditure and requirements vary, depending on the illness or trauma. The increase in energy expenditure above basal needs is about 10% for elective operations, 10–30% for trauma, 50–80% for sepsis, and 100–200% for burns (depending on the extent of the wound). Metabolic energy can be derived from carbohydrates, proteins, or fats.
Carbohydrate Metabolism
Carbohydrates are the body's primary fuel source under usual conditions, accounting for 30–40% of total caloric intake. Each gram of enteric carbohydrate provides 4 kilocalories (kcal) of energy. Parenterally administered carbohydrates (eg, intravenous dextrose) yield 3.4 kcal per gram.
Carbohydrate digestion is initiated by the action of salivary amylase, and absorption is generally completed within the first 1.0–1.5 m of the small intestine. Salivary and pancreatic amylases cleave starches into oligosaccharides on contact.
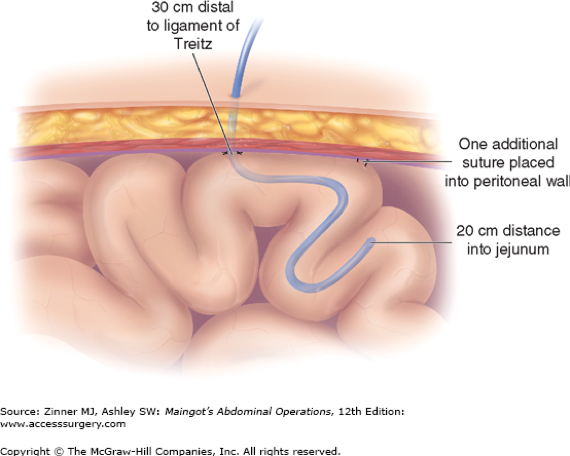
Feeding enterostomy: Enterostomy in the high jejunum may be utilized for feeding purposes in malnourished patients, either before or after major surgical procedures.
Surface oligosaccharidases then hydrolyze and transport these molecules across the GI tract mucosa. Deficiencies in carbohydrate digestion and absorption are rare in surgical patients. Pancreatic amylase is abundant, and maldigestion of starch does not usually occur, even in patients with limited pancreatic exocrine function. Patients with diseases such as celiac sprue, Whipple's disease, and hypogammaglobulinemia often have generalized intestinal mucosal flattening and consequent oligosaccharidase deficiency and diminished uptake of carbohydrate.
Board Review Questions
1. Choose the one best response to this question.
A 35-year-old trauma victim with malabsorption requires hyperalimentation. The patient's injuries include a stable nondisplaced fracture of the third thoracic vertebra, a closed head injury, multiple upper and lower extremity fractures and bilateral pulmonary contusions requiring ventilatory support. Which of the following are the most appropriate site and type of venous access in this patient?
| A. bilateral antecubital fossae, 18G peripheral intravenous catheters |
| B. femoral vein, central venous catheter (CVC) |
| C. dorsum of one foot, single 16G peripheral intravenous catheter |
| D. subclavian vein, CVC |
2. Choose the one best response to this question.
A 35-year-old male trauma patient is being considered for extubation from a 10-day course of ventilatory support after a motor vehicle accident in which he suffered several hollow viscus injuries requiring an exploratory laparotomy. The patient has been receiving parenteral nutrition and currently has a tidal volume of 400 mL and a respiratory rate of 40 breaths/min. What changes in his hyperalimentation may improve this patient's minute ventilation?
| A. adding long-acting insulin to the mixture |
| B. increasing the proportion of glucose calories |
| C. decreasing the total volume with a more concentrated solution |
| D. increasing the proportion of fat calories |
| E. adding fat soluble vitamins A, D, E, and K |
3. Choose the one best response to this question.
A 45-year-old male with alcoholic liver disease and short gut syndrome was previously on chronic parenteral nutrition. He has been switched to an elemental enteral diet for the past 6 months, which has been poorly tolerated. He has complained of generalized weakness for several months and now has erythematous, scaly and symmetrical lesions on his upper extremities, stomatitis, and glossitis. What is the most appropriate treatment for these symptoms?
| A. addition of fat soluble vitamins A, D, E, and K |
| B. thiamine replacement |
| C. niacin replacement |
| D. change to a lactose-free enteral feed |
| E. addition of tincture of opium |
Answers
1. The correct answer is D. subclavian vein, CVC.
2. The correct answer is D. increasing the proportion of fat calories.
3. The correct answer is C. niacin replacement.
Read more about Nutrition in the Surgical Patient on AccessSurgery in Schwartz's Principles of Surgery.

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.