Patellar Tendinopathy

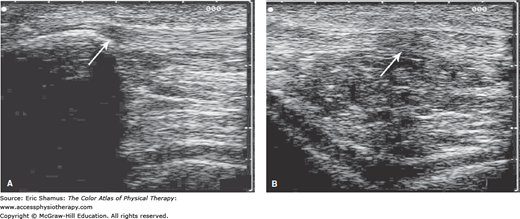
Scenario: A 21-year-old, 6′5″, 190 pound, Division II male collegiate basketball player, with no previous history of knee and/or patellofemoral pathology, reports to the athletic training/sports medicine facility complaining of bilateral anterior knee pain. He states the pain began approximately 2 weeks ago, with the highest incidence of pain occurring in the morning after a weight-training session. About 3 days ago, the pain became constant and has impacted his training. He reported that as part of his off-season conditioning, he has increased strength training (e.g., squats, leg extensions, etc.) and plyometric activities (e.g., box jumps, bounding, etc.) aimed toward increasing power output and vertical jump height. His training over the previous 6 weeks focused on the lower extremity, with 30 to 45 minutes per day of cardiovascular training (e.g., running, cycling) to supplement the 4 days per week of Olympic lifting techniques and plyometric training. He admitted he does not focus on pretraining dynamic warm-ups and performs limited postactivity stretching, but did use ice post activity a few times to manage his pain. The patient presents with no obvious deformity or signs of Osgood–Schlatter disease; no obvious laxity or instability at the patellofemoral joint. Manual muscle testing (eccentric break test) WNL for knee and hip with exception of 4/5 grading: bilateral hip flexion, internal rotation, external rotation, and knee extension. He has a positive Thomas test and positive Ely test, suggesting muscular tightness in his iliopsoas and rectus femoris bilaterally. During gait analysis, he presents with an early heel rise during terminal stance, suggesting tight gastroc-soleus (Achilles tendon). Kinetic chain dysfunction from muscular tightness was further evident during an observed body-weight squat. Radiologic findings include X-rays (negative) and musculoskeletal diagnostic ultrasound (positive for inflammation).
Question: What are some patient education deficits that should be addressed with this patient?
A. Footwear recommendations, short healing time, activity limitations such as no driving.
B. Training errors including stretching and warmup, proper healing time (may be longer), and footwear recommendations.
C. Proper healing time, weight loss,
D. Training errors including stretching and warmup, activity limitations such as no driving, weight loss.
Answer with rationale: B. Training errors including stretching and warmup, proper healing time (may be longer), and footwear recommendations. Patient stated he has not been completing the proper warmup procedures, including stretching. These warmup procedures are crucial to help prevent patellar tendinopathy, and the patient should be educated on including them during rehabilitation and when he returns to full competition. Patient’s footwear should be evaluated for support and corrected if necessary. Patient should be educated that this injury may take a longer time to heal, and that he should make sure not to return to full participation too soon, or reinjury may occur.
For more information see Chapter 198: Patellar Tendinopathy in The Color Atlas of Physical Therapy.
Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.