Dermatology Question of the Week: Medical Mysteries

Question:
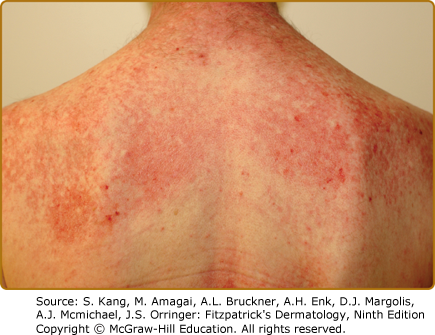
A 60-year-old female presents with intractable scalp pruritus. She had been given clobetasol solution, ketoconazole shampoo, fluocinolone oil, and over the counter anti-dandruff shampoos by her previous dermatologist. None of the treatments have helped. On exam, you note that the scalp has a pink color diffusely with minimal scale and also note the following finding seen in the photograph below.
Other than the pruritic rash on the back and scalp, her review of systems is negative. You perform a punch biopsy on the back which shows interface dermatitis and you subsequently order the appropriate lab work up. Which of the following antibodies would suggest the patient has a more indolent disease course that will respond better to treatment and has a lower risk of internal involvement?
Answer choices:
A. Anti-TIF1-gamma
B. Anti-Mi-2
C. Anti-NXP2
D. Anti-SSA
E. Anti-MDA5
Rationale: Dermatomyositis is a systemic autoimmune condition that frequently affects the skin and/or muscle. Cutaneous findings include shawl sign (as noted in the photograph above), V-neck sign, nail fold changes including ragged cuticles and abnormal capillaries, heliotrope sign (violaceous periorbital patches), Gottron papules, Gottron sign (papules on the elbows/knees), Holster sign (poikiloderma on the thighs), and scalp erythema. Some of the less commonly observed findings include ulcerations, flagellate erythema, calcinosis cutis, and an ovoid palatal patch. Dermatomyositis can often be associated with interstitial lung disease or malignancy. Autoantibodies, while not always present, can help stratify risk of malignancy, pulmonary involvement, and speed of progression. Severe scalp pruritus, as in the patient above, is a very common presenting sign that is frequently overlooked or misdiagnosed.
Correct answer: B
Anti-Mi-2 antibodies are seen in approximately 15% of adult dermatomyositis. Patients typically present with cutaneous disease with mild muscle disease. Anti-Mi-2 is associated with a lower incidence of malignancy and is not typically associated with progressive interstitial lung disease. These patients tend to respond well to treatment.
Incorrect answers:
A. Anti-TIF1-gamma is associated with diffuse cutaneous disease and frequently seen in amyopathic disease. The rate of cancer identification in these patients ranges from 19-100% depending on the publication; however, in a recent systematic review the odds ratio of cancer was 9.37 in patients with TIF1-gamma positivity. Furthermore, the malignancy is typically detected within the 3 years before or after diagnosis of dermatomyositis.
C. Similar to anti-TIF-1-gamma, Anti-NXP2 antibodies are associated with an increased risk of malignancy. In both adult and juvenile forms, calcinosis cutis is frequently observed.
D. Anti-SSA is seen in SCLE, neonatal lupus, and Sjogren syndrome. It is not typically associated with dermatomyositis and does not fit with this patient’s clinical presentation.
E. Anti-MDA5 antibodies are associated with severe cutaneous ulcerations in addition to interstitial lung disease which can frequently have a rapid progression.
Additional information at Chapter 62 - Dermatomyositis
References:
Best M, Molinari N, Chasset F, Vincent T, Cordel N, Bessis D. Use of Anti-transcriptional Intermediary Factor-1 Gamma Autoantibody in Identifying Adult Dermatomyositis Patients with Cancer: A Systematic Review and Meta-analysis. Acta Derm Venereol. 2019 Mar 1;99(3):256-262. doi: 10.2340/00015555-3091
Khanna U, Galimberti F, Li Y, Fernandez AP. Dermatomyositis and malignancy: should all patients with dermatomyositis undergo malignancy screening? Ann Transl Med. 2021 Mar;9(5):432. doi: 10.21037/atm-20-5215.
Fiorentino DF, Chung LS, Christopher-Stine L, Zaba L, Li S, Mammen AL, Rosen A, Casciola-Rosen L. Most patients with cancer-associated dermatomyositis have antibodies to nuclear matrix protein NXP-2 or transcription intermediary factor 1γ Arthritis Rheum. 2013;65:2954–2962. doi: 10.1002/art.38093
Oldroyd A, Sergeant JC, New P, McHugh NJ, Betteridge Z, Lamb JA, Ollier WE, Cooper RG, Chinoy H. The temporal relationship between cancer and adult onset anti-transcriptional intermediary factor 1 antibody-positive dermatomyositis. Rheumatology (Oxford) 2019;58:650–655. doi: 10.1093/rheumatology/key357.
Marzęcka M, Niemczyk A, Rudnicka L. Autoantibody Markers of Increased Risk of Malignancy in Patients with Dermatomyositis. Clin Rev Allergy Immunol. 2022 Oct;63(2):289-296. doi: 10.1007/s12016-022-08922-4.

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.