Dermatology Question of the Week: Medical Mysteries

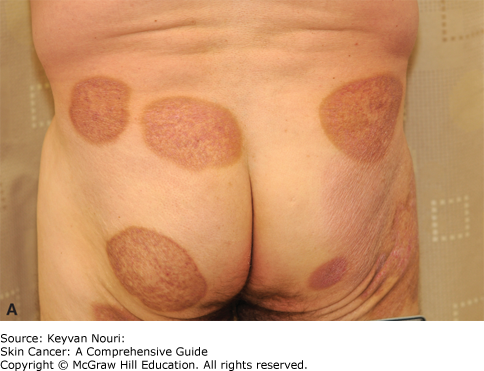
A 65-year-old male presents with a five-year history of intermittent, somewhat pruritic, erythematous patches on his buttocks and thighs shown below.
A skin biopsy performed three months ago showed lymphocytic infiltration in the epidermis with atypical lymphocytes. He has <10% body surface area involvement, limited to patches and plaques. No lymphadenopathy or systemic symptoms are noted. Flow cytometry of peripheral blood does not demonstrate circulating atypical lymphocytes.
Which of the following statements regarding this diagnosis are correct?
(hint: more than one answer choice may be correct)
A. Biopsy from a sun-exposed site is generally recommended
B. Skin-directed therapy is the first-line treatment for this stage of the disease
C. Systemic chemotherapy is recommended to prevent disease progression
D. A second skin biopsy should always be performed for staging purposes
E. This condition has a chronic, indolent course in most cases
F. The disease is characterized predominantly by CD8+ T cells
Rationale:
Mycosis fungoides (MF) is a type of cutaneous T-cell lymphoma. MF can present with a wide variety of phenotypes including pink patches/plaques, nodules/tumors, erythroderma, or a hypopigmented variant seen in patients with skin of color. Diagnosis relies on clinical and histopathological findings. Staging depends on the extent of skin involvement, lymph node status, and presence of systemic disease. With <10% body surface area involvement limited to patches and plaques and no systemic involvement, the patient is classified as stage IB (<10% BSA with patches and plaques). Early-stage MF generally has a chronic, indolent course.
Correct answers:
B. Skin-directed therapy is the first-line treatment for this stage of the disease
Early-stage MF is primarily managed with skin-directed therapies such as topical corticosteroids, phototherapy, or topical nitrogen mustard. These approaches are typically effective in controlling symptoms and disease progression while minimizing systemic side effects.
E. Mycosis fungoides has a chronic, indolent course in most cases
In the early stages, MF often progresses slowly over many years or even decades. Prognosis is generally favorable for patients with limited skin involvement. Goals of care are symptom control and maintaining quality of life.

Incorrect answers:
A. Biopsy from a sun-exposed site is generally recommended
Biopsy from a "double-covered" area such as the buttocks, axilla, or breast/inframammary region is generally recommended. Natural sunlight can inhibit these malignant T-cells which can make the infiltrate less prominent on histology and diagnosis more difficult. For this reason, selecting a biopsy site that is less likely to be impacted by sunlight is important to achieving the correct diagnosis.
C. Systemic chemotherapy is recommended to prevent disease progression
Systemic chemotherapy is reserved for advanced-stage disease, including tumor-stage MF, erythrodermic MF, or Sézary syndrome. It is not appropriate for early-stage MF due to its significant toxicity and lack of efficacy in early disease stages. In fact, MF is different than most lymphomas in that most first-line treatments are immunomodulatory such as Bexarotene (a retinoid), Mogamolizumab (CCR4 inhibitor), and Romidepsin (HDAC inhibitor) rather than traditional chemotherapy.
D. A second skin biopsy should always be performed for staging purposes
While repeat biopsies are frequently needed if the diagnosis is uncertain, they are not routine for staging. Staging is primarily based on clinical examination, BSA estimation, lymph node assessment, and blood tests to evaluate systemic involvement. A staging chart is shown below.
Table 119-7 Staging System for Mycosis Fungoides and Sézary Syndrome
| STAGE | T (TUMOR) | N (LYMPH NODE) | M (METASTASES) | B (BLOOD) |
|---|---|---|---|---|
| IA | T1 | N0 | M0 | B0 or B1 |
| IB | T2 | N0 | M0 | B0 or B1 |
| IIA | T1 or T2 | N1 or N2 | M0 | B0 or B1 |
| IIB | T3 | N0-N2 | M0 | B0 or B1 |
| III | T4 | N0-N2 | M0 | B0 or B1 |
| IIIA | T4 | N0-N2 | M0 | B0 |
| IIIB | T4 | N0-N2 | M0 | B1 |
| IVA1 | T1-T4 | N0-N2 | M0 | B2 |
| IVA2 | T1-T4 | N3 | M0 | B0-B2 |
| IVB | T1-T4 | N0-N3 | M1 | B0-B2 |
T1, patch/plaque on ≤10% of body surface; T2, patch/plaque on ≥10% of body surface; T3, skin tumor(s); T4, erythroderma; N0, normal nodes; N1, palpable nodes without clear histologic evidence of lymphoma (for N1 and N2, “a” or “b” may be added for either no [a] or detection [b] of a T-cell clone by Southern blot or polymerase chain reaction [PCR] analysis); N2, palpable nodes, histologic evidence of lymphoma, node architecture preserved; N3, palpable nodes with histologic evidence of lymphoma, effacement of node architecture; M0, no visceral involvement; M1, histologically confirmed visceral involvement. B0, ≤5% Sézary cells (for B0 and B1, “a” or “b” may be added for either no [a] or detection [b] of a T-cell clone by Southern blot or PCR analysis); B1, >5% Sézary cells but either less than 1.0 K/µL absolute Sézary cells or absence of a clonal rearrangement of the TCR or both; clonal rearrangement of the TCR in the blood and either 1.0 K/µL or more Sézary cells or one of the following 2: (a) increased CD4+ or CD3+ cells with CD4/CD8 of 10 or more or (b) increase in CD4+ cells with an abnormal phenotype (>40% CD4+/CD7− or >30% CD4+/CD26−).
F. The disease is characterized predominantly by CD8+ T cells
Mycosis fungoides is typically characterized by a malignant population of CD4+ T cells.
Additional reading at Fitzpatrick's Dermatology Chapter 119: Cutaneous Lymphoma and Skin Cancer: Chapter 12: Cutaneous Lymphomas & Leukemias

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.