Dermatology Question of the Week: Deductive Dermpath

Question:
A 46-year-old male presents with a 6-month history of rash on his lower legs pictured below. He is otherwise well without any known medical conditions. Given the unclear etiology, you perform a biopsy showing the histology below. Which of the following would explain the findings seen on histology?

Answers:
A. AA fibril protein
B. AL protein
C. Aker protein
D. Keratin 5
E. Beta-2-microglobulin
Rationale:
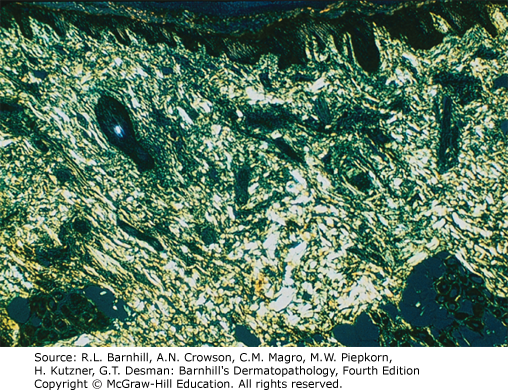
Differentiating between the different types of amyloid is important clinically and for test-taking purposes. Amyloidosis can be divided into systemic primary, systemic secondary, and localized. Genetic and hemodialysis-associated forms also exist. There are three main forms of localized cutaneous amyloidosis: macular, lichen, and nodular amyloidosis. Amyloid has green birefringence with polarized light when stained with Congo red as shown below.
Correct answer: B AL protein
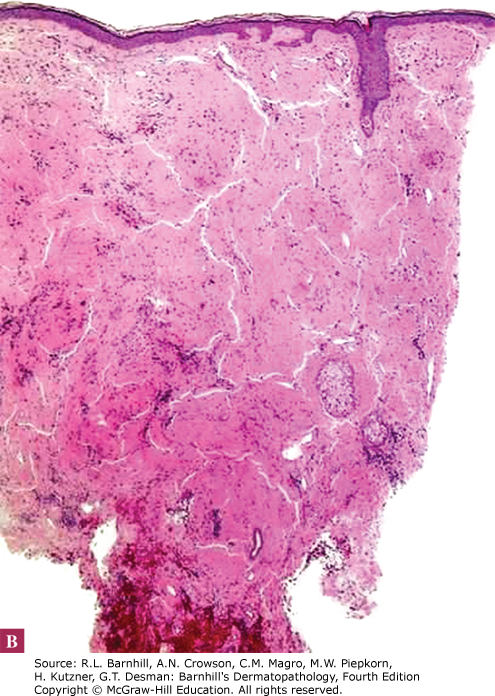
Nodular amyloidosis presents clinically with brown-pink papules or nodules typically on the lower extremities/acral surfaces and the face. Histologically, amyloid deposits are found in the dermis, can extend into the subcutis, and are frequently found within vessel walls. Nodular amyloidosis is differentiated from the other two forms of localized cutaneous amyloidosis by the presence of AL protein derived from immunoglobulin light chains. Nodular amyloidosis has an approximately 7% risk of progression to systemic amyloidosis; therefore, these patients should be monitored closely. Additionally, nodular amyloidosis can be associated with autoimmune conditions, particularly Sjogren's syndrome, and patients should be screened accordingly.
Incorrect answers:
A. AA amyloid is found in secondary systemic amyloidosis. AA amyloid is derived from serum amyloid A (SAA). Deposition in the skin is rare as this form typically involves the kidneys, spleen, liver, adrenals, and heart.
C and D. Macular amyloidosis and lichen amyloidosis contain Aker protein that is derived from keratinocyte tonofilaments, particularly keratin 5. Macular amyloidosis most commonly presents as hyperpigmented patches on the upper back. Lichen amyloidosis presents with pruritic papules and plaques on extensor surfaces. Both macular and lichen amyloidosis are thought to be the result of chronic scratching and subsequent trauma to basal keratinocytes resulting in the release and degradation of cytokeratins. Lichen amyloidosis can also be seen in association with MEN2a.
E. Beta-2-microglobulin deposition is seen in hemodialysis-associated amyloidosis. This typically does not present with skin involvement however some reports of cutaneous nodular amyloidosis with beta-2-microglobulin have been reported. This does not fit with our clinical vignette as the patient is otherwise well and not on hemodialysis.
Additional reading at Fitzpatrick's Dermatology Chapter 125: Amyloidosis and Barnhill's Dermatopathology Chapter 16: Deposition Disorders

Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.