A 35-week gestational age infant is born by cesarean delivery to a mother with placenta previa.

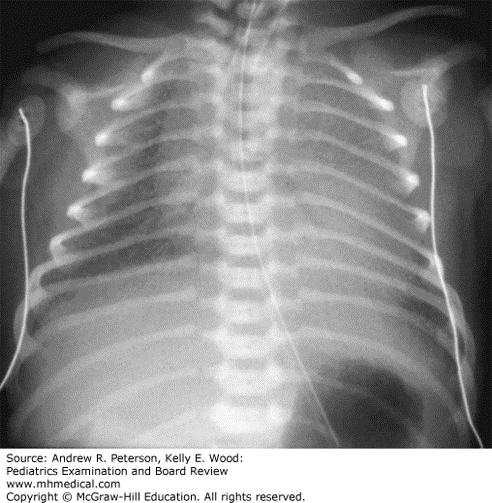
A 35-week gestational age infant is born by cesarean delivery to a mother with placenta previa. The infant girl is vigorous after delivery, with Apgar scores of 8 and 8. She is brought to her mother’s chest. Fifteen minutes later the NICU team is called because the infant is experiencing worsening respiratory distress with tachypnea, retractions, and mild grunting respirations. She is placed on nasal CPAP and admitted to the NICU. The infant continues to be tachypneic, at 80 breaths per minute, has mild retractions, and requires 40% FiO2 on CPAP. Her chest radiograph shows approximately 7-rib expansion with ground glass opacities throughout all lung fields.
(Reproduced with permission from Tintinalli JE, Stapczynski JS, Ma OJ, et al: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8th ed. McGraw-Hill Education, Inc., 2016. Fig 107-2.)
You are asked to update her family. You tell them:
A: This is most consistent with neonatal pneumonia and sepsis. You will start antibiotics immediately and she will recover in several days to a week.
B: This is most consistent with respiratory distress syndrome resulting from surfactant deficiency related to prematurity. She may need to be intubated for surfactant administration.
C: This is most consistent with transient tachypnea of the newborn and fluid retention exacerbated by the cesarean delivery without labor. She will improve in the next 24 hours.
D: This is most consistent with meconium aspiration. She will improve within days to weeks.
E: None of the above.
Explanation: The correct answer is “B.” This infant has persistent distress on CPAP with rising oxygen and evidence of respiratory distress syndrome on chest radiograph with decreased lung expansion and findings consistent with surfactant deficiency. Although respiratory distress syndrome is most common in very preterm infants, many late preterm infants of less than 37 weeks’ gestation have surfactant deficiency, especially those who have not had spontaneous labor. If clinical symptoms continue to worsen, oxygen needs increase, or gas exchange is poor as evidenced by respiratory acidosis on blood gas measurements, then this infant should be intubated and surfactant administered through the endotracheal tube.
From: Pediatrics Examination and Board Review, Fetus and Newborn > Case 14.10




Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.