Week 17 Q&A
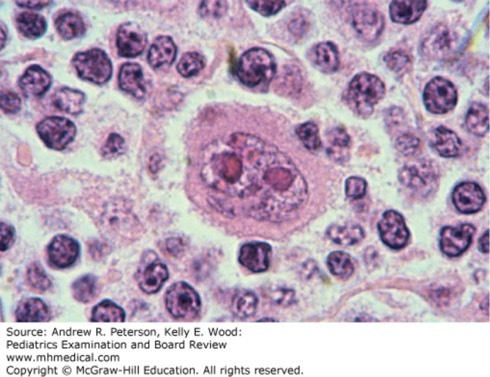
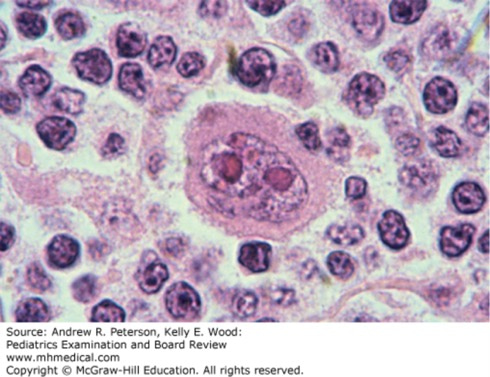
Onset of symptoms was 6 months ago, with increasing pruritus, flushing, and night sweats. She occasionally felt increasing pressure in her chest while lying down, and was having difficulty taking deep breaths. Physical examination was remarkable for posterior cervical lymphadenopathy, 10 cm on the right and 5 cm on the left. Coarse crackles were appreciated in the lower lung fields bilaterally. Saturation of peripheral hemoglobin by oxygen (SpO2) was 86% on room air. A CBC revealed hemoglobin of 10.6 g/dL, white blood cell count (WBC) 15 ×103/mm3 (differential: neutrophils 15%, lymphocytes 73%, monocytes 8%, eosinophils 4%), and platelets 382 ×103/mm3. An excisional lymph node biopsy reveals the finding shown in figure below.
This finding was noted on excisional biopsy of the patient’s enlarged lymph node (Case 6). (Reproduced with permission from Kaushansky K, Lichtman MA, KBeutler E, et al: Williams Hematology, 8ed. McGraw-Hill Education, Inc., 2010. Fig 98-34.
Of the following, the most likely diagnosis is:
A. Acute lymphoblastic leukemia.
B. Hodgkin lymphoma.
C. Infectious mononucleosis.
D. Diffuse large B-cell lymphoma.
E. Systemic lupus erythematosus.
The correct answer is “B.” The figure exhibits a classic binucleate Reed-Sternberg cell, with the typical “owl’s eyes” appearance to the nucleoli. It is pathognomonic for Hodgkin lymphoma (HL), although not all HL will present with this finding on biopsy [7]. In a patient with lymphadenopathy that is worrisome for malignancy, such as the patient in the vignette, note that consultation with a pediatric surgeon is recommended to ensure that excisional biopsy is obtained; the sampling error associated with needle core biopsy increases the chance of false-negative results, need for re-biopsy, and delay in diagnosis and treatment. Apart from this piece of data, this is a teenage patient with several months of lymphadenopathy, fever, and cough, with other chest symptoms suggestive of a chest mass. The quality of symptoms may overlap with those of infectious mononucleosis (option “C”), but the duration is atypical, and the CBC did not report atypical lymphocytes that would be suspicious for Epstein-Barr virus infection. Similarly, the largely normal CBC does not raise suspicion for acute lymphoblastic leukemia (ALL, option “A”); one should expect ALL to exhibit marked cytopenias and possibly leukocytosis. The biopsy result is inconsistent with lupus (option “E”). The age of the patient, with constitutional illness and symptoms consistent with a chest mass, should be clues for HL. Non-Hodgkin lymphomas (NHL, option “D”) might also have similar presenting findings, although among pediatric patients, NHL is more common in younger children and HL is more common in adolescents and young adults. Hodgkin lymphoma is curable with chemotherapy. In the past, patients with splenic involvement have undergone splenectomy as part of their therapy, although this is not commonly recommended for pediatric patients. Asplenic patients are at increased risk of infection with encapsulated organisms; it is recommended that splenectomy be delayed until 23-valent pneumococcal and meningococcal vaccinations can be administered. Prompt attention to fevers in splenectomized patients, with blood culture and empiric antibiotic therapy during a 48-hour sepsis rule-out, is recommended.
Source: Peterson AR, Wood KE. Pediatrics Examination and Board Review; 2017.





Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.