Tarsal Tunnel Syndrome

A 27-year-old male recreational runner/jogger presents with right ankle and foot pain and numbness of 2 weeks duration. The patient reports spraining his ankle 6 months ago when he turned his ankle inward while jogging on an uneven surface. He sustained a sprain to his medial ankle that resolved uneventfully in 2 to 3 weeks. Upon returning to running/jogging, the patient noted stiffness and generalized right lower-extremity weakness but denied ankle or leg pain. Patient reports that he returned to his typical jogging mileage of more than 35 miles/week with 2 weeks of return to jogging. At this time, he reports medial ankle and foot paresthesia/numbness beneath his medial malleolus that travels into the medial arch and plantar aspect of his foot and heel. Numbness/paresthesia is increased shortly after initiating jogging and is notable with standing and walking, especially if the patient wears sandals or flip-flops. Upon palpation, the patient reports pain and tenderness inferior to his medial malleolus. The patient has a positive Tinel sign with testing inferior to medial malleolus. Weakness noted for flexion of the big toe.
Question: Based on these findings, what nerve is affected in this patient, and what is the best treatment option for the affected nerve?
Potential answers:
A. Lateral plantar nerve. Corticosteroid injection first, then surgery as soon as possible.
B. Posterior tibial nerve. Conservative treatment first for symptoms, and if no improvement, surgical measures to release the nerve.
C. Medial plantar nerve. No conservative treatments, surgery to release nerve as soon as possible.
D. Common fibular nerve. Conservative treatment first for symptoms, and if no improvement, surgical measures to release the nerve.
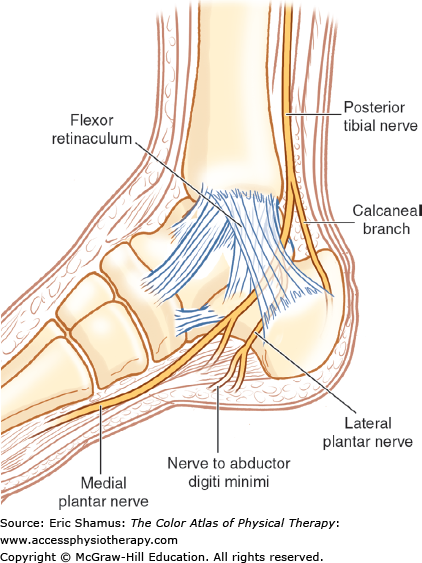
Answer with rationale: B. Posterior tibial nerve. Conservative treatment first for symptoms, and if no improvement, surgical measures to release the nerve. The posterior tibial nerve is the only nerve running through the tarsal tunnel, and the main nerve on the medial side of the ankle. Also, the posterior tibial nerve innervates flexor digitorum longus and flexor hallucis longus, both of which are mentioned as weak and sensory deficient with this patient. Conservative management of symptoms should help to alleviate some of the effects, and can be successful in coordination with patient education. With severe and/or chronic tarsal tunnel syndrome, if no improvement with 6 to 12 months of conservative measures, surgery should be considered.
For more information please see Chapter 227: Tarsal Tunnel Syndrome in The Color Atlas of Physical Therapy.
Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.