GUILLAIN–BARRÉ SYNDROME

Scenario: A 25-year-old woman is brought into the emergency department (ED) after sinking to the ground during a volleyball match. Her teammate notes that she had been stumbling and was starting to have more difficulty with her serve for the past week. On arrival, she can no longer raise her legs and labors to adjust herself in bed. She has also begun to complain of shortness of breath. She denies fever but states that 3 weeks ago the entire team suffered from abdominal cramps and diarrhea after a championship cookout. The patient denies previous health problems. Her temperature is 36.6°C (98°F); heart rate, 50 beats/min; respiration rate, 26 breaths/min; and blood pressure, 90/60 mmHg. She can only keep her arms up against gravity for 5 seconds, and her hands are limp. She has slight movement of her legs with decreased sensation of pain and fine touch in her lower legs. Her reflexes are absent. She has no skin lesions. Her heart and lung examinations are unremarkable except for bradycardia and poor inspiratory effort. MRI of the brain and spine is normal. It is suspected that the patient has Guillain-Barre.
Question: What is nadir, and what physical therapy interventions should be prioritized once the patient reaches this point?
Potential answers:
- Nadir is the initial presentation of symptoms. Passive ROM and positioning should be prioritized at this point in the syndrome progression.
- Nadir is the point when the syndrome progression has reached its most intense and then stabilized. Bodyweight exercises and functional mobility, sitting balance, and antigravity ROM should be prioritized at this point in the syndrome progression.
- Nadir is the point when symptoms are progressively intensifying. Passive ROM and positioning should be prioritized at this point in the syndrome progression
- Nadir is the point when the syndrome damage has proven to be permanent. Functional muscle control exercises, sitting and standing balance, and closely monitored aerobic exercises should be prioritized at this point in the syndrome progression.
Answer with rationale: 2. Nadir is the point when the syndrome progression has reached its most intense and then stabilized. Bodyweight exercises and functional mobility, sitting balance, and antigravity ROM should be prioritized at this point in the syndrome progression.
Clinical nadir in reference to Guillain-Barre is the point when progressive symptoms have reached their worst, and then begin to stabilize. This point usually occurs at around 2 to 4 weeks after symptom onset.
Bodyweight exercises and functional mobility should be prioritized to begin recovery after an extended period of rest and limited mobility. Functional mobility assists the patient in regaining some level of independence for daily activities. Bodyweight exercises are a good place to start reconditioning.
Sitting balance and antigravity ROM should be prioritized because they play an integral role in functional mobility, and in daily activities.
Standing tolerance should also be prioritized here for functional mobility purposes, and energy conservation methods to help the patient increase ability to get through their day without exhausting themselves.
For more information see Chapter 88 Guillain-Barre Syndrome in the Color Atlas of Physical Therapy.
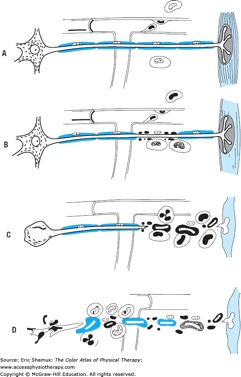
Diagram of probable cellular events in acute inflammatory polyneuropathy (Guillain–Barré syndrome). A. Lymphocytes attach to the walls of endoneurial vessels and migrate through the vessel wall, enlarging and transforming as they do so. At this stage no nerve damage has occurred. B. More lymphocytes have migrated into the surrounding tissue. The first effect on the nerve is breakdown of myelin, the axon being spared (segmental demyelination). This change appears to be mediated by the mononuclear exudate, but the mechanism is uncertain. C. The lesion is more intense, polymorphonuclear leukocytes are present as well as lymphocytes. There is interruption of the axon in addition to myelin sheath damage; as a result, the muscle undergoes denervation atrophy, and the nerve cell body shows central chromatolysis. If the axonal damage is distal, the nerve cell body will survive, and regeneration and clinical recovery are likely. If, as in D, axonal interruption has occurred proximally because of a particularly intense root or proximal nerve lesion, the nerve cell body may die and undergo dissolution. In this situation, there is no regeneration, only the possibility of collateral reinnervation of muscle from surviving motor fibers. (From Asbury AK, Arnason BGW, Adams RD. The inflammatory lesion in acute idiopathic polyneuritis. Medicine [Baltimore]. 1969;48:173.)
Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.