He has not been febrile today; however, he recently recovered from what his mother thought was the flu. His vital signs are HR 140 bpm, RR 40, BP 70/50 mm Hg, and T 37.5°C (99.5°F). The emergency department physician obtains IV access, sends off laboratory studies and a blood culture, administers a total of 40 mL/kg of isotonic fluid, and administers broad-spectrum IV antibiotics. The patient is now noted to be more tachycardic, with increased work of breathing, and pulses that are difficult to palpate.

What is the most likely cause of this child’s decompensation?
A. Septic shock.
B. Viral bronchiolitis.
C. Bacterial pneumonia.
D. Systemic inflammatory response syndrome (SIRS).
E. Congestive heart failure.
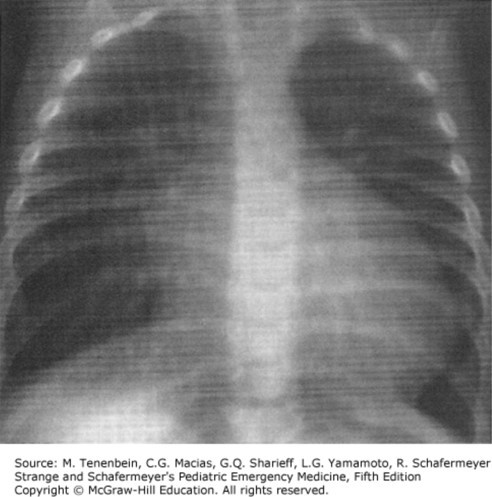
The correct answer is “E.” When approaching a patient in shock, remember to continually reassess after each therapy. Although fluid resuscitation is the appropriate initial management for any patient in shock, the reassessment helps to determine what type of shock the patient is experiencing. After fluid resuscitation, the presence of rales, hepatomegaly, worsening tachycardia, and worsening perfusion are all signs consistent with cardiogenic shock. In patients with septic shock or systemic inflammatory response syndrome (SIRS), one would not expect a worsening clinical status following aggressive fluid resuscitation. In a patient with viral bronchiolitis or bacterial pneumonia, work of breathing may continue to progress with fluid resuscitation; however, worsening perfusion would not be expected. Once the diagnosis of cardiogenic shock is suspected, a 2-dimensional echocardiogram is needed to confirm the diagnosis. This will help determine if the patient is suffering from impaired systolic or diastolic function (eg, myocarditis), or tamponade physiology (eg, pericardial effusion). With impaired systolic function epinephrine can augment contractility. Recall that epinephrine does increase myocardial oxygen demand and has the potential to lead to myocardial ischemia and infarction. If impaired diastolic function is present, milrinone can help relaxation and filling. Recall that milrinone will also lead to vasodilation and must be used cautiously in the hypotensive patient. The triad of tachycardia, jugular venous distention, and narrowed pulse pressure is tamponade physiology until proven otherwise. The definitive diagnosis is clinically made, and the therapy of choice is echocardiogram-guided pericardiocentesis if a pericardial effusion is to blame. Aggressive diuresis in the setting of tamponade physiology could result in significantly diminished systemic venous return and cardiac arrest.
Sources:
Question & Explanation: Peterson AR, Wood KE. Pediatrics Examination and Board Review. New York, NY: McGraw-Hill Education; 2017.





Create a Free MyAccess Profile
AccessMedicine Network is the place to keep up on new releases for the Access products, get short form didactic content, read up on practice impacting highlights, and watch video featuring authors of your favorite books in medicine. Create a MyAccess profile and follow our contributors to stay informed via email updates.